Management of Hip Fractures in the Elderly Case Study
Hip fractures are seen in many orthopaedic practices. The American Academy of Orthopaedic Surgeons (AAOS) Clinical Practice Guideline Management of Hip Fractures in the Elderly is a summary of the available literature designed to help guide the surgeon and other qualified physicians in the management of this condition. The full document is available online at http:// www.aaos.org/research/guidelines/ HipFxGuideline.pdf. The following case presentation highlights how these guidelines can be helpful to the clinician when deciding the course of treatment.History and Physical Examination
An 81-year-old woman presents to the emergency department after slipping on the ice in her driveway. She reports right hip pain and an inability to bear weight. She has no prior history of hip pain and is ambulatory with the use of a cane. She lives with her husband and performs all activities of daily living independently. Her medical history includes mild senile dementia, hypertension, stable coronary artery disease, and a history of transient ischemic attack. She is currently on low-dose aspirin, clopidogrel, metoprolol, lisinopril, and pravastatin.
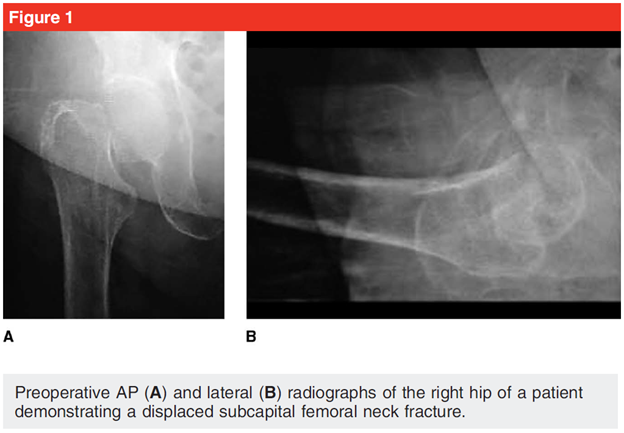
Physical examination of the right hip shows a positive log roll test and demonstrates pain with range of motion. The patient’s right leg is flexed and shortened. The skin over the hip and thigh is intact with no abrasions, and the knee and ankle are non-tender, with pain-free range of motion. The leg is also neurovascularly intact with good sensation, capillary refill, and pulses in the foot. Radiographs demonstrate a displaced subcapital femoral neck fracture of the right hip (Figure 1). The patient receives an ultrasoundguided fascia iliacus regional nerve block in the emergency department for pain control and is admitted to the hospital for treatment of her hip fracture. Preoperative traction is not used (per the AAOS guideline, “moderate evidence does not support routine use of preoperative traction for patients with a hip fracture”), but the patient is placed on bed rest with use of intermittent pneumatic compression devices. Adequate pain relief is achieved with acetaminophen following the administration of a regional block, which was used to minimize the risk of delirium.1,2 The patient is evaluated by the medicine service; it is determined that she is at acceptable risk for surgery. It is recommended that surgery not be delayed despite the patient’s use of aspirin and clopidrogrel.3 (The AAOS guideline states that “limited evidence supports not delaying hip fracture surgery for patients on aspirin and/or clopidogrel.”)
The orthopaedic surgeon has a discussion with the patient and family regarding the overall long-term prognosis of possible decreased mobility and independence as a result of the hip fracture. The discussion also includes the possibility of mortality. After considering nonsurgical treatment measures, the patient makes an informed decision to proceed with surgery based on the quality of life and mobility benefits associated with this method of treatment. The surgeon also discusses with the patient the option of a total hip arthroplasty for the benefit of improved function and long-term results.4 Following consideration of the patient’s relatively low functional demands and lack of pre-existing hip arthritis, as well as the surgeon’s relative inexperience with performing total hip arthroplasty, the decision is made to proceed with hemiarthroplasty because the merits of a more complicated and expensive procedure do not outweigh the associated inherent risks. (The Academy guideline states that “moderate evidence supports a benefit to total hip arthroplasty in properly selected patients with unstable [displaced] femoral neck fractures.”)
Management
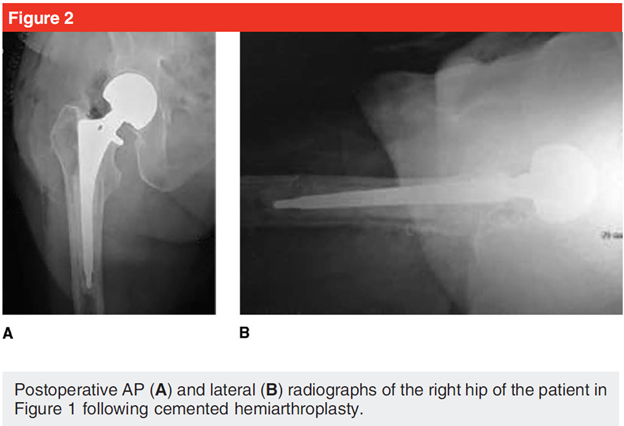
It is decided to have the patient proceed to surgery on the day of admission because of the improved mobility and mortality outcomes associated with early surgery.5 (Moderate evidence indicates that hip fracture surgery within 48 hours of admission is associated with better outcomes.) The anesthesiologist and patient decide on a general anesthetic after discussing the relative risks and benefits of both local and general anesthetic techniques, as well as the similar outcomes. The patient has a history of difficult spinal anesthesia because of lumbar spine disease. (The AAOS Guideline strongly recommends the use of regional anesthesia “unless a clear and compelling rationale for an alternative approach is present,” which is the situation in this case.) The patient undergoes cemented unipolar hemiarthroplasty without complications.6,7 The surgeon performs an anterolateral approach to minimize the risk of dislocation.8 (Per the guideline, “moderate evidence supports higher dislocation rates with a posterior approach.”) Postoperative radiographs demonstrate good position of the prosthesis without evidence of periprosthetic fracture (Figure 2).
Postoperatively, the patient is mobilized. Weight-bearing exercises are introduced as tolerated with physical and occupational therapy. She is placed on low-molecular-weight heparin and continues on clopidrogrel and intermittent pneumatic compression devices because of the high risk of venous thromboembolic events in this patient population. Her admission albumin level was low; the nutrition service is consulted. The patient is started on nutritional supplements following surgery to improve her protein levels and caloric intake (a moderate-grade recommendation). In addition, she is found to be vitamin D deficient, with a vitamin D level of 23 ng/ml (normal, .30 ng/ml); calcium and vitamin D supplementation are initiated.
Pain is initially well controlled after surgery because of the long-acting regional nerve block. A multimodal pain regimen is also used (a stronggrade recommendation), including perioperative celecoxib, long-acting oral narcotics, acetaminophen, and tramadol, thus minimizing narcotic use to avoid delirium.9 The patient’s hemoglobin level decreases to 8.1 g/dL postoperatively; however, her blood pressure is stable. Although she experiences some transient lightheadedness and tachycardia, this improves with hydration; a transfusion is not given because of the relative associated risks.10 (In the guideline, strong evidence supports a blood transfusion threshold of no higher than 8 g/dL in asymptomatic postoperative hip fracture patients unless a clear and compelling rationale for an alternative approach is present.)
The patient progresses well during her hospital stay, and an interdisciplinary care program is used with discharge planning, rehabilitation, and posthospital services. (Strong evidence supports the use of an interdisciplinary care program in patients with mild to moderate dementia to improve functional outcomes.) This care program coordinates her transition from inpatient care to subacute rehabilitation and, ultimately, back to her own home with home care. She is prescribed continued supplementation of calcium and vitamin D and is referred for outpatient evaluation of osteoporosis because of her high risk of further fragility fractures (both graded as moderate recommendations in the guideline). She is later started on zoledronic acid treatment.11 Aggressive physical and occupational therapy is used throughout the continuum of care, with a focus on improving balance, mobility, functional activities of daily living, strength, and fall prevention.
Outcome
Three months following her fracture, the patient regains independence; however, her mobility decreases, causing her to require the long-term use of a walker.
References
1. Rosen JE, Chen FS, Hiebert R, Koval KJ: Efficacy of preoperative skin traction in hip fracture patients: A prospective, randomized study. J Orthop Trauma 2001; 15(2):81-85.
2. Mouzopoulos G, Vasiliadis G, Lasanianos N, Nikolaras G, Morakis E, Kaminaris M: Fascia iliaca block prophylaxis for hip fracture patients at risk for delirium: A randomized placebocontrolled study. J Orthop Traumatol 2009;10(3):127-133.
3. Hossain FS, Rambani R, Ribee H, Koch L: Is discontinuation of clopidogrel necessary for intracapsular hip fracture surgery? Analysis of 102 hemiarthroplasties. J Orthop Traumatol 2013;14(3):171-177.
4. Keating JF, Grant A, Masson M, Scott NW, Forbes JF: Randomized comparison of reduction and fixation, bipolar hemiarthroplasty, and total hip arthroplasty: Treatment of displaced intracapsular hip fractures in healthy older patients. J Bone Joint Surg Am 2006;88(2): 249-260.
5. McGuire KJ, Bernstein J, Polsky D, Silber JH: The 2004 Marshall Urist award: Delays until surgery after hip fracture increases mortality. Clin Orthop Relat Res 2004;428:294-301.
6. Taylor F, Wright M, Zhu M: Hemiarthroplasty of the hip with and without cement: A randomized clinical trial. J Bone Joint Surg Am 2012;94(7):577-583.
7. Davison JN, Calder SJ, Anderson GH, et al: Treatment for displaced intracapsular fracture of the proximal femur: A prospective, randomised trial in patients aged 65 to 79 years. J Bone Joint Surg Br 2001;83(2):206-212.
8. Sköldenberg O, Ekman A, Salemyr M, Bodén H: Reduced dislocation rate after hip arthroplasty for femoral neck fractures when changing from posterolateral to anterolateral approach. Acta Orthop 2010; 81(5):583-587.
9. Kang H, Ha YC, Kim JY, Woo YC, Lee JS, Jang EC: Effectiveness of multimodal pain management after bipolar hemiarthroplasty for hip fracture: A randomized, controlled study. J Bone Joint Surg Am 2013;95(4): 291-296.
10. Carson JL, Terrin ML, Noveck H, et al; FOCUS Investigators: Liberal or restrictive transfusion in high-risk patients after hip surgery. N Engl J Med 2011;365(26): 2453-2462.
11. Lyles KW, Colón-Emeric CS, Magaziner JS, et al; for the HORIZON Recurrent Fracture Trial: Zoledronic acid in reducing clinical fracture and mortality after hip fracture. N Engl J Med 2007;357:a40967.
