Diagnosis and Treatment of Osteochondritis Dissecans Case Study
IntroductionOsteochondritis dissecans (OCD) in children and adults is a relatively rare condition of the distal aspect of the femur. It is difficult to determine the true incidence and prevalence of this disorder because many of the lesions are asymptomatic and may be found incidentally on a radiograph obtained for other purposes. Although the AAOS Diagnosis and Treatment of Osteochondritis Dissecans work group reviewed all of the English-language literature on this condition, the actual incidence in our population remains unclear.
The AAOS Clinical Practice Guideline Diagnosis and Treatment of Osteochondritis Dissecans is a summary of the available high quality research designed to help guide the clinician on the evaluation and management of these conditions. The following case presentation is designed to highlight how the guideline can be used by the clinician in deciding the course of treatment.
History
A 15-year-old boy presents reporting pain in his right knee for the past 18 months. He is an avid soccer player but does not recall having had any specific injury. He has no swelling, clicking, or locking of his knee. However, his pain is such that he cannot play an entire game.
Physical Examination
The patient does not have an effusion of his knee but does have tenderness over the medial femoral condyle. No provocative maneuvers reproduce his pain. A review of the literature does not suggest that there are any specific clinical findings in OCD lesions.
Imaging
The patient undergoes radiography and MRI of the knee (Figure 1).
Figure 1
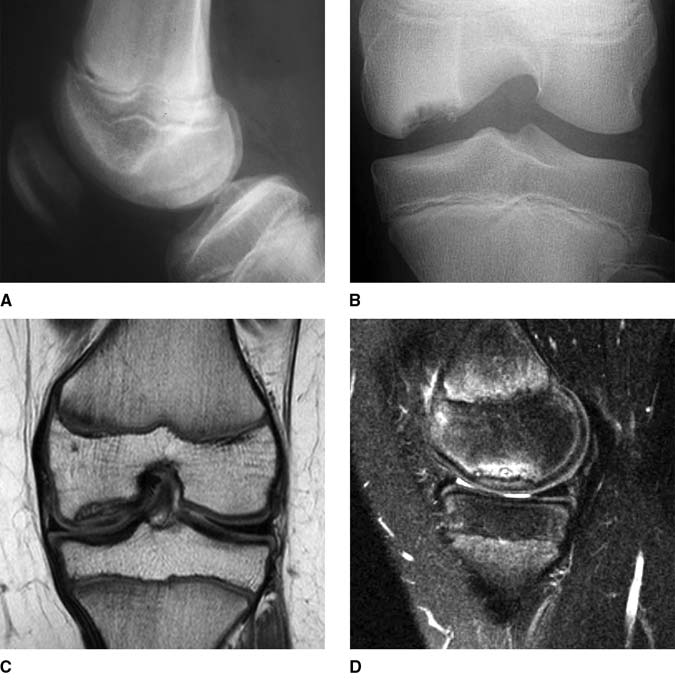
A 15-year-old boy presented with pain in his right knee for the past 18 months. A, Preoperative lateral radiograph. B, Tunnel/notch radiograph of the distal femur. Coronal T1-weighted (C) and sagittal T2-weighted (D) magnetic resonance images of the right knee.
The recommendation in the AAOS Clinical Practice Guideline to obtain and interpret radiographs and MRI of the knee is rated as weak. There is an unknown incidence of bilaterality of OCD; however, we are unable to find quality evidence to recommend imaging of the contralateral knee. There is no conclusive evidence that other imaging studies (eg, CT, nuclear bone scans) are useful adjuncts in the evaluation of OCD.
Treatment
The AAOS Guideline evaluated four separate patient populations: Skeletally immature patients with stable lesions, skeletally immature patients with unstable lesions, skeletally mature patients with stable lesions, and skeletally mature patients with unstable lesions. The options for treatment, as in most orthopaedic conditions, are nonsurgical or surgical. Although there is a belief that nonsurgical treatment (eg, casting, bracing, splinting, unloader braces, electrical or ultrasound bone stimulators, activity restriction) would be an option, no prospective studies have determined the efficacy of any of these methods. In fact, no one treatment method for either the stable or unstable lesions has demonstrated superiority. Because of the possibility of degenerative changes, the work group suggested that patients with unstable or displaced lesions be offered the option of surgery.
This patient undergoes a 6-week course of activity modification but no bracing, splinting, or casting. He continues to have pain, and there is no change in the radiographic appearance of the lesion. The patient, family, and surgeon opt for surgical management consisting of intraepiphyseal, extra-articular drilling. Other techniques have been used, including transarticular drilling, with good results in level IV studies. The extra-articular technique has the potential advantage of not perforating the articular cartilage, whereas the intra-articular technique does not require the use of image intensification. However, the evidence does not favor either of these techniques.
In this technique, AP and lateral fluoroscopic views are taken of the knee after diagnostic arthroscopy is performed. A central 0.062 Kirschner wire (K-wire) is inserted, and a series of K-wire perforations (15 to 20) is performed around this central pin (Figure 2).
Figure 2

The patient in Figure 1. A, AP radiograph demonstrating central pin placement. B, Lateral radiograph demonstrating placement of two pins. C, Intraoperative photograph demonstrating arthroscopic and radiographic pin placement.
Postoperative Protocol
The work group could not ascertain whether any particular postoperative regimen or physical therapy protocol has any influence on the outcome of nonsurgical or surgical management. In the absence of evidence, however, many different techniques, including non–weight bearing for a certain period (eg, 6 weeks), full weight bearing to strengthening, proprioception training, and advanced rehabilitation, have been suggested. In the present case, the patient is kept touch-down weight bearing for 6 weeks. Figure 3 demonstrates the radiographic and MRI outcomes at 3 months postoperatively.
At 3 months, the patient was released to full sporting activity. Based on the evidence available, there is no one specific treatment that would lead to this radiographic outcome.
Figure 3
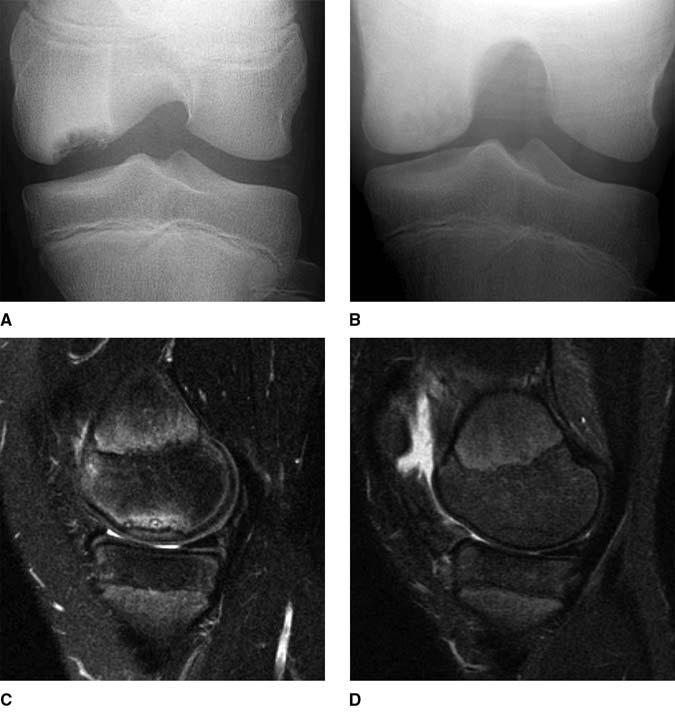
AP radiographs demonstrating the tunnel view preoperatively (A) and 3 months postoperatively (B). Sagittal magnetic resonance images obtained preoperatively (C) and 3 months postoperatively (D).
Summary
The AAOS Clinical Practice Guideline on osteochondritis dissecans of the knee presents few conclusive recommendations on the diagnosis and treatment of children and adults with stable and unstable lesions. Many different evaluation and treatment modalities have been used, although few in a prospective, randomized manner. The guideline does suggest using MRI to evaluate the lesion. However, all other recommendations are either inconclusive or required consensus grading. This guideline will serve as a roadmap for further investigation into this vexing condition.
