Treatment of Symptomatic Osteoporotic Spinal Compression Fractures Case Study
IntroductionSymptomatic osteoporotic spinal compression fractures are seen in many orthopaedic practices. The American Academy of Orthopaedic Surgeons (AAOS) Clinical Practice Guideline, “The Treatment of Symptomatic Osteoporotic Spinal Compression Fractures,” is a summary of the available literature designed to help guide the surgeon and other qualified physicians in the management of this condition. The following case presentation highlights how these guidelines can be helpful to the clinician when deciding the course of treatment.
History
A 66-year-old woman presents with a 2-day history of sudden back pain after having lifted a vacuum cleaner from her closet. She reports having had a bone density test done the week before, with a T score of -2.5. She denies any recent weight loss or recent back pain and was in good overall health before this incident.
Physical Examination
The clinical history is consistent with an osteoporotic spinal compression fracture. The patient is tender to percussion in the midlumbar region and has pain noted with movement. There is no local kyphotic deformity, and she is neurologically intact.
Imaging Studies
AP and lateral radiographs reveal compression of the L3 vertebral body (Figure 1). To define the acuity of the process, magnetic resonance images also are obtained.
Figure 1

Lateral radiographic view of the lumbar spine demonstrating evidence of L3 compression fracture.
Treatment
The patient is diagnosed with an osteoporotic vertebral body compression fracture without neurologic compromise. Treatment decisions should be made in light of all circumstances presented by the patient. Decisions regarding the applicable treatment and procedures are made by relying on mutual communication between the patient, physician, and other health care providers.
The AAOS guidelines show a Moderate strength recommendation in the use of calcitonin for 4 weeks following the onset of an acute osteoporotic compression fracture. Also, there is a Weak recommendation on the use of ibandronate and strontium ranelate to prevent additional symptomatic fractures in patients who present with signs and symptoms correlating with an acute vertebral compression fracture.
The AAOS has taken an Inconclusive stance regarding bed rest, the use of complementary and alternative medicine, or the use of opioids/analgesics in patients who present with correlating clinical signs and symptoms of an acute osteoporotic compression fracture who are neurologically intact. Further, there is a Weak recommendation regarding use of an L2 nerve root block in patients with an L3 or L4 compression fracture.
The AAOS also has taken an Inconclusive stance regarding brace treatment, prescription of a supervised or unsupervised exercise program, and the use of electrical stimulation in patients who present with an osteoporotic spinal compression fracture on imaging with correlating clinical signs and symptoms and who are neurologically intact.
The AAOS has a Strong recommendation against the use of vertebroplasty for patients who present with an acute osteoporotic spinal compression fracture and are neurologically intact.
Weak recommendations for kyphoplasty exist should patients with osteoporotic spinal compression fractures who are neurologically intact not improve with nonsurgical management (Figures 2 through 4).
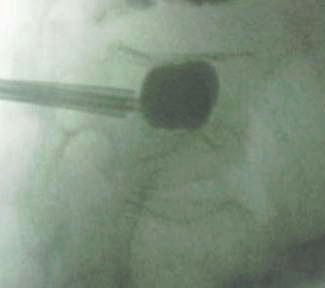
Figure 2

Lateral radiographic view of the L3 vertebra. A pedicle cannula is in place, and a deflated balloon is in position for kyphoplasty.
Figure 3
Lateral radiographic view of the L3 vertebra with the balloon being inflated to create a cavity for cement insertion.
Figure 4

Lateral radiographic view of the L3 vertebra demonstrating uniform filling to the end plates of the cavity.
Outcome and Resolution
This patient was treated nonsurgically for 4 weeks but did not have resolution of severe back pain symptoms; therefore, she desired to proceed with surgical treatment. A kyphoplasty was performed (Figures 2 through 4). Subsequently, this patient reported good relief of her back pain and maintenance of her normal neurologic status, and she has been able to resume her normal activities. She has also been referred to a rheumatologist, who is medically treating her osteoporosis.
Currently, the AAOS is unable to recommend either for or against improvement of kyphotic angle in patients with osteoporotic spinal vertebral fractures. Should a patient with an osteoporotic spinal vertebral fracture also have a neurologic deficit, the AAOS is unable to recommend for or against any specific treatment.
Based on the evidence available, the AAOS recommendations on the treatment of symptomatic osteoporotic spinal compression fractures range from Inconclusive to Strong. Further studies are needed to better define appropriate treatment and timing for treatment. However, knowledge of the present guidelines is helpful for surgeons and other health care providers who treat and counsel patients with symptomatic osteoporotic spinal compression fractures.
