Treatment of Glenohumeral Joint Osteoarthritis Guideline Case Study
A 75 year old RHD female presents with a six month history of left shoulder pain. She denies any previous trauma to the shoulder. The pain is not present all of the time. It can bother her during sleep. She feels that over time she is unable to reach as high as she previous could. There are times when the shoulder can lock up on her. It will also make a grinding noise intermittently with use of the arm. She describes the pain primarily over the front of the shoulder. She has not tried any NSAIDS, nor has she engaged in physical therapy or received any cortisone injections.Physical exam of the left shoulder: skin was intact throughout. No evidence of effusion at the glenohumeral joint. She demonstrates intact axillary nerve autogenous zone to soft touch and 5/5 deltoid strength. Forward elevation: 140-180 with pain throughout the arc of motion on right. External rotation: 25-40. Internal rotation: buttock-L2. Drop arm maneuver produces pain with audible and palpable crepitus. There is pain to palpation over the anterior glenohumeral joint. No pain over the greater tuberosity.
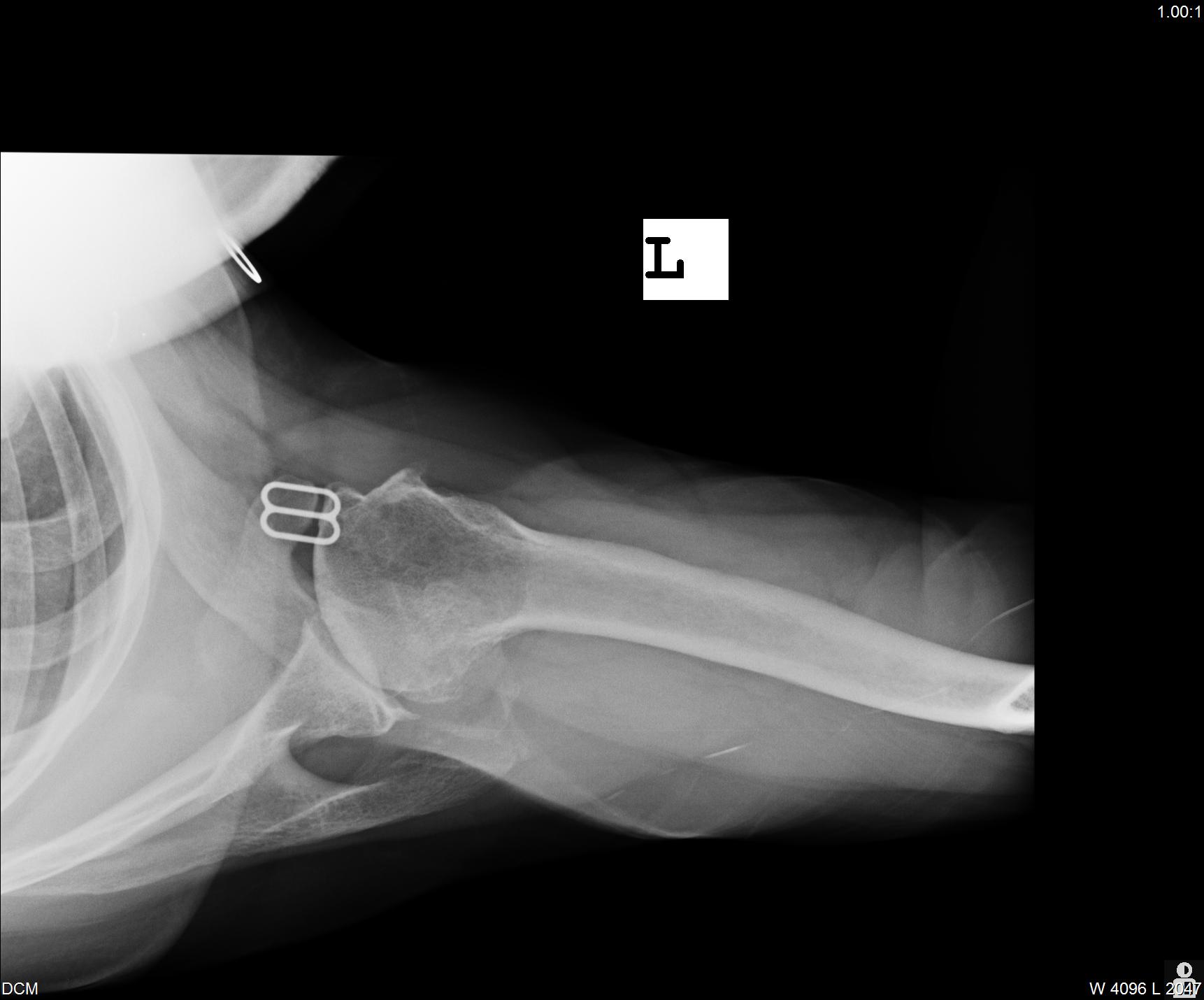
X-rays (Figure 1) demonstrate severe narrowing of the glenohumeral joint space. There is no evidence of superior migration of the humeral head. There are associated inferior humeral head osteophytes. On the axillary there is concentric wear of the glenoid.
Figure 1
.jpg)

Pre-Op Ax Pre-Op AP.2 Pre-Op Scap Y
The patient elects to try ibuprofen and PT. Three months later she returns to the office. She states that she completed the entire course of PT and while she felt she may have gained some motion in her shoulder, her pain did not change. The ibuprofen did not seem to provide much pain relief and bothered her stomach. Her exam is essentially unchanged. She elects to undergo a cortisone injection after discussing the risks and benefits.
She returns to the office seven months later. The injection gave her excellent pain relief for six months. Given the success of the first injection she requests a second. She returns to office in four months. Unfortunately, this injection only provided three months of relief. A discussion follows regarding further injections. She elects to have a third injection understanding that no further cortisone injections would be recommended.
When she returns to the office two months later her symptoms are returned to her baseline, if not somewhat worse. Her activities of daily are becoming more challenging. Washing the dishes has even become taxing. She now has almost nightly difficulty with sleeping. She feels that her quality of life has become significantly affected and would like to discuss the next step in treatment of her glenohumeral arthritis.
The patient elects to undergo a total shoulder arthroplasty. Her postoperative x-rays are shown in Figure 2. She is discharged to home on post- operative day 1. At her first postoperative visit she asks if she will need physical therapy.
Figure 2
.jpg)

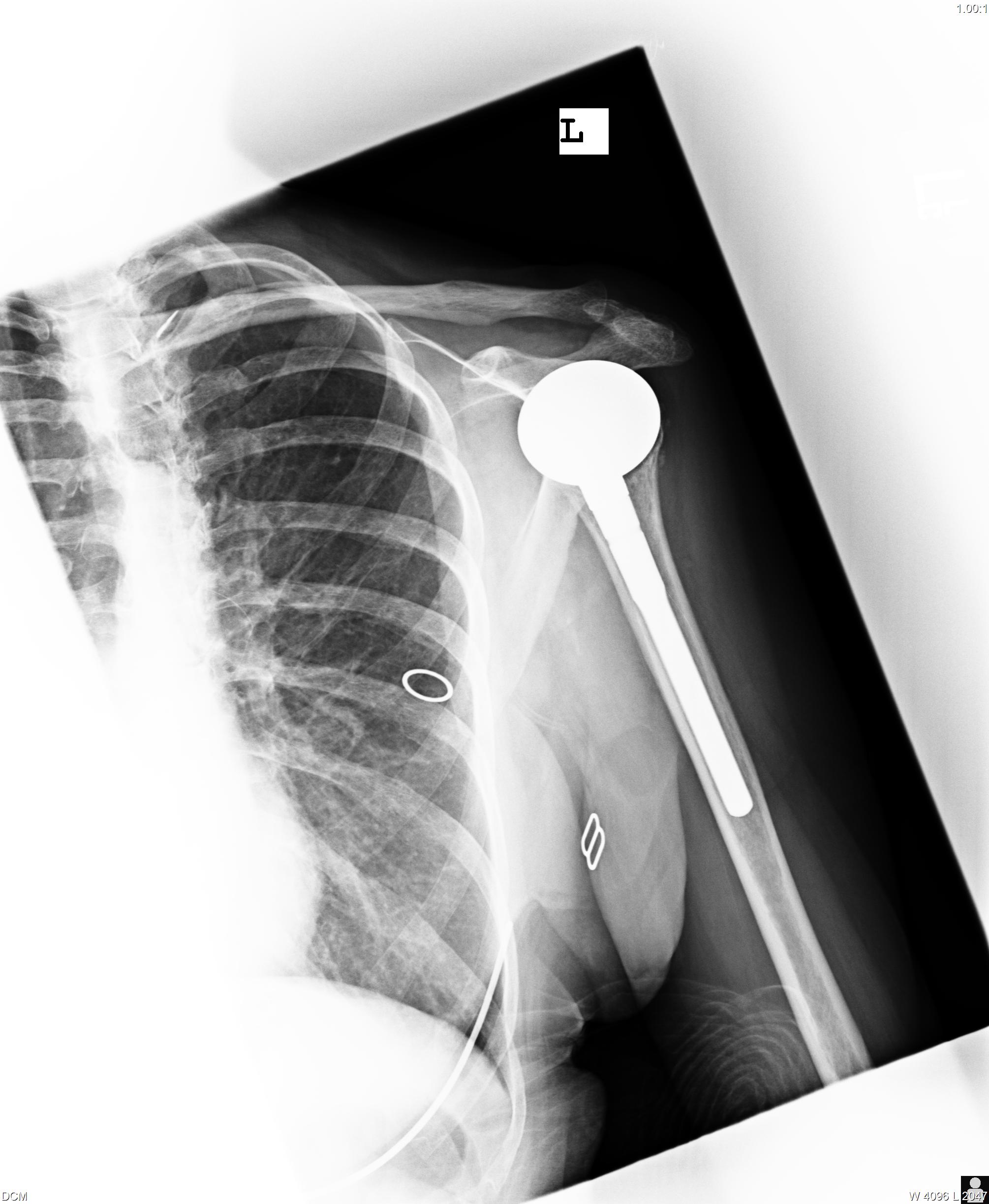
Post-Op Ax Post-Op AP Post-Op Scap Y
The patient elects to pursue physical therapy. She wears a sling for six weeks postoperatively. At her six week postoperative visit the sling is discontinued. She continues with organized therapy until her three month postoperative visit: at which time she has full functional range of motion and is pain free.
- Gartsman GM, Roddey TS, Hammerman SM: Shoulder arthroplasty with or without resurfacing of the glenoid in patients who have osteoarthritis. J Bone Joint Surg Am 2000; 82 (1):26-34.
- Lo IK, Litchfield RB, Griffin S, Faber K, Patterson SD, Kirkley A: Quality of life outcome following hemiarthroplasty or total shoulder arthroplasty in patients with osteoarthritis: A prospective, randomized trial. J Bone Joint Surg Am 2005;87(10):2178-2185.
